
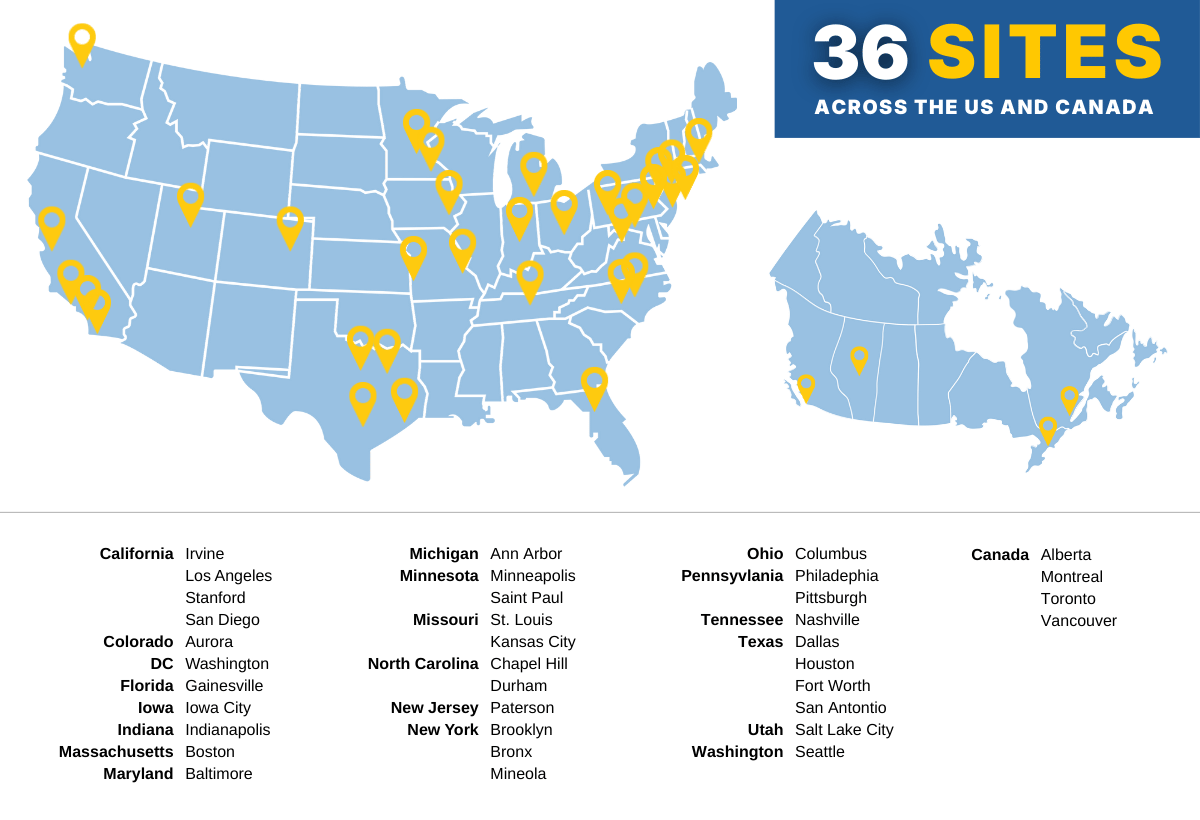
The Prader-Willi Syndrome Clinical Investigation Collaborative (PWS-CLIC) is a nationwide network of expert clinicians dedicated to improving care for and advancing clinical research for people with Prader-Willi syndrome (PWS). With 36 participating sites across the United States and Canada, the PWS-CLIC connects families and clinicians with providers who have experience caring for individuals with PWS and a shared commitment to learning from every patient.
The goal of the PWS-CLIC is simple but powerful: improve outcomes for people with PWS across the lifespan by strengthening clinical care today and accelerating the development of better treatments for tomorrow.
The PWS-CLIC aims to improve the quality of medical care and clinical research for individuals with PWS through collaborative investigation and data-driven practices. By connecting experts across multiple medical disciplines, the collaborative works to identify key clinical questions, share insights and observations, and generate evidence that supports informed, consistent, and effective care.
For families, the PWS-CLIC offers access to knowledgeable providers who understand the complexities of PWS across the lifespan. For clinicians, it offers a collaborative professional network and the infrastructure needed to ask—and answer—important clinical questions.
One of the most important ways the PWS-CLIC works toward its mission is by learning from every patient, so care can be improved for all. A deeper understanding of the natural history of PWS—the typical patterns, variations, and challenges experienced across the lifespan—helps clinicians anticipate medical concerns earlier and work to reduce their frequency and severity.
To do this effectively, clinicians need the ability to “compare notes,” identify data trends, and understand how often certain complications occur across a large, representative PWS population. To support this, the PWS-CLIC, in partnership with FPWR, launched a PWS-CLIC Database to complement the caregiver-entered data in the Global PWS Registry.
The CLIC database is a secure, cloud-based electronic data capture system where CLIC clinicians enter de-identified clinical data (with all personal identifiers removed) for individuals with PWS. The database allows experts to:
When families participate, they help ensure the data reflects the full diversity of the PWS community and supports the continued growth of expert, informed care.
By pooling this clinical data and tracking outcomes over time, clinicians can better understand which approaches to care are most effective for managing the complex medical needs associated with PWS.
This clinician-entered data complements the caregiver-reported information collected through the Global PWS Registry, creating a more complete picture of health, medical management, and quality of life. Families who participate in the CLIC database are encouraged to link their CLIC data with their Global PWS Registry record, further strengthening the impact of both efforts.
University of California, Irvine - Irvine, CA
Dr. Virginia Kimonis, Pediatrics
Children's Hospital of Los Angeles - Los Angeles, CA
Dr. Alaina Vidmar, Pediatric Endocrinology
Stanford University - Stanford, CA
Dr. Diane Stafford, Pediatric Endocrinology
Rady Children's Hospital - San Diego, CA
Dr. Lynne Bird, Clinical Genetics
Children's Hospital Colorado - Aurora, CO
Dr. Shawn McCandless, Pediatric Genetics
Children's National Hospital - Washington, DC
Dr. Elizabeth Estrada, Pediatric Endocrinology
University of Florida - Gainesville, FL
Dr. Jennifer Miller, Pediatric Endocrinology
University of Iowa - Iowa City, IA
Dr. Eva Tsalikian, Pediatric Endocrinology
Indiana University - Indianapolis, IN
Dr. Nancy Johnson, Pediatrics
Boston Children's Hospital - Boston, MA
Dr. Amy Fleischman, Pediatric Endocrinology
Johns Hopkins University - Baltimore, MD
Dr. Ann Scheimann, Pediatrics
University of Michigan - Ann Arbor, MI
Dr. Daniel Shumer, Pediatric Endocrinology (site PI)
Dr. Nellie Hani, Pediatric Endocrinology (co-I)
University of Minnesota Masonic Children's Hospital - Minneapolis, MN
Dr. Bradley Miller, Pediatric Endocrinology
Children's Minnesota - Saint Paul, MN
Dr. Jen Abuzzahab, Pediatric Endocrinology
SSM Health Cardinal Glennon Children's Hospital - St. Louis, MO
Barbara Whitman, PhD, Pediatrics (co-I),
Dr. Jennifer Heithaus, Developmental Pediatrics (co-I)
Children's Mercy Kansas City - Kansas City, MO
Dr. Kelsee Halpin, Pediatric Endocrinology (Site PI),
Dr. Emily Paprocki, Pediatric Endocrinology (co-I)
University of North Carolina - Chapel Hill, NC
Dr. Jennifer Law, Pediatric Endocrinology (Site PI),
Dr. Elizabeth Jalazo, Pediatrics (co-I)
Duke University - Durham, NC
Dr. Olga Gupta, Pediatric Endocrinology and Obesity Medicine
St. Joseph's University Medical Center - Paterson, NJ
Dr. Katerina Harwood, Pediatric Endocrinology
Maimonides Medical Center - Brooklyn, NY
Dr. Deepan Singh, Psychiatry
Albert Einstein College of Medicine - Bronx, NY
Dr. Eric Hollander, Psychiatry and Behavioral Sciences
NYU Langone Health - Mineola, NY
Dr. Jorge Mejia-Corletto, Pediatric Endocrinology
Nationwide Children's Hospital - Columbus, OH
Dr. Kathryn Obrynba, Pediatric Endocrinology
Children's Hospital of Philadelphia - Philadelphia, PA
Dr. Ben Yerys, PhD, Psychology (site PI),
Dr. Adda Grimberg, Pediatric Endocrinology (co-I),
Dr. Raghuram Prasad, Psychiatry (co-I)
University of Pittsburgh - Pittsburgh, PA
Dr. Ann Johansson, PhD, DNP, Medical Genetics
Vanderbilt University - Nashville, TN
Dr. Ashley Shoemaker, Pediatric Endocrinology
Endocrine Associates of Dallas - Dallas, TX
Dr. Heidi Shea, Adult and Pediatric Endocrinology
Texas Children's Hospital - Houston, TX
Dr. Kathy Hwu, Pediatrics
Cook's Children's Medical Center - Fort Worth, TX
Dr. Sani Roy, Pediatric Endocrinology (Site PI),
Dr. Keisha Shaheed, Sleep Medicine (co-I)
Children's Hospital of San Antonio - San Antonio, TX
Dr. Elizabeth Roeder, Pediatric Genetics
University of Utah - Salt Lake City, UT
Dr. Dave Viskochil, Pediatric Genetics
Seattle Children's Hospital - Seattle, WA
Dr. Isabella Niu, Pediatric Endocrinology (Site PI),
Dr. Melinda Pierce, Pediatric Endocrinology (co-I)
University of Alberta - Edmonton, AB
Dr. Andrea Haqq, Pediatrics
BC Children's Hospital - Vancouver, BC
Dr. Sanjukta Basak, Pediatric Endocrinology
The Hospital for Sick Children - Toronto, ON
Dr. Jill Hamilton, Pediatrics
CHU Sainte-Justine - Montreal, QC
Dr. Nathalie Alos, Pediatrics (Site PI);
Dr. Cheri Deal, Pediatric Endocrinology (co-I)
A core strength of the PWS Clinical and Research Expert Consortium is the ability to translate shared clinical experience into meaningful insights that improve care. By pooling data from PWS clinics across the country, the PWS-CLIC is beginning to answer important clinical questions that individual centers cannot address on their own.
As participation in the CLIC and the CLIC database continues to grow, this body of work will expand, providing an increasingly robust evidence base to inform clinical care, guide future research, and support the development of improved treatments for individuals with PWS.

 |
Dr. Diane Stafford is a Clinical Professor of Pediatrics at Stanford University School of Medicine in the Division of Endocrinology and Diabetes. She has been providing care to children and young adults with PWS for over 20 years and has a particular interest in disorders of puberty seen in the syndrome. |
 |
Dr. Shawn E. McCandless (Chair of the CLIC Executive Committee) is a Professor of Pediatrics, and the Section Head for Genetics and Metabolism at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado. He is past President of the Society for Inherited Metabolic Disorders (SIMD). His research has focused on inborn errors of metabolism (IEM) and Prader-Willi syndrome (PWS), including publicly and industry-funded clinical trials for children and adults with IEMs and PWS. After training with Dr. Suzanne Cassidy, he has been the Medical Director of PWS multi-disciplinary clinics in North Carolina, Ohio, and now in Colorado. He is board-certified in Pediatrics (1992), Clinical Genetics (1999), and Clinical Biochemical Genetics (2005). He is a fellow of the American Academy of Pediatrics and of the American College of Medical Genetics. |
 |
Dr. Dave Viskochil has focused his research on the molecular genetics of neurofibromatosis type 1 (NF1). Under the mentorship of John Carey and Ray White, he was a recipient of the Young Investigator Award from the National Neurofibromatosis Foundation (now CTF; Children’s Tumor Foundation) in 1988. He is Medical Director for the University of Utah Genetics Counselor Training Program and Director of the Medical Genetics Training Program at the University of Utah. He serves as the Director of the Prader-Willi Syndrome Clinic at the University of Utah. He oversees care of MPS (mucopolysaccharidosis) Disorders at the University of Utah and serves on the International Board of Advisors for the MPS I Registry. He provides genetics services for the TSC (tuberous sclerosis complex) Clinic at the University of Utah. His career focus has shifted to the implementation of clinical trials for rare disorders. |

|
Dr. Ann Scheimann is a member of the full-time faculty within the Department of Pediatrics/Division of Pediatric Gastroenterology at Johns Hopkins School of Medicine and continues to see patients with Prader-Willi Syndrome at Johns Hopkins and through the Prader-Willi Syndrome Clinic at Texas Children's Hospital. Dr. Scheimann's focus of research interest has been in nutrition and obesity with special areas of interest in Prader-Willi Syndrome and nonalcoholic fatty liver disease. She has authored or co-authored to date approximately 90 peer-reviewed publications in addition to book chapters, and meeting presentations. |

|
Dr. Sani Roy is a pediatric endocrinologist at Cook Children’s Medical Center. She did her endocrine fellowship training at The Children’s Hospital of Philadelphia, where she was heavily involved in growth and obesity research. After arriving at Cook Children’s in 2016, Dr. Roy spent several years working to develop a multidisciplinary center for Prader-Willi syndrome. The Multidisciplinary Prader-Willi Wellness, Education, and Research Center (MPoWER) formally launched in 2022, and she currently serves as the MPoWER Center Director. Dr. Roy holds an Endowed Chair for Prader-Willi syndrome from Cook Children’s, and she serves on the Board of Advisers for the Global Prader-Willi Syndrome Registry and is on the Executive Committee for PWS-CLIC. Dr. Roy is actively involved in clinical trials and in collaborative projects to better understand and treat the endocrine and multidisciplinary aspects of PWS. |

|
Dr. Lynne M Bird is a Professor of Clinical Pediatrics at University of California, San Diego and a clinical geneticist with 30 years of practice experience at Rady Children’s Hospital San Diego. She has served as Medical Director of a multidisciplinary Prader-Willi syndrome clinic for the past 20 years and has extensive PWS clinical trial experience including studies of beloranib, carbetocin, livoletide, GLWL-01, cannabidiol, RGH-706, diazoxide choline extended release, and transcutaneous vagus nerve stimulator.
|
The Foundation for Prader-Willi Research (federal tax id 31-1763110) is a nonprofit corporation with federal tax exempt status as a public charity under section 501(c)(3).



The mission of FPWR is to eliminate the challenges of Prader-Willi syndrome through the advancement of research and therapeutic development.
Copyright © 2020. All Rights Reserved. Terms of Use. Privacy Policy. Copyright Infringement Policy. Disclosure Statement.