 Mental health and behavioral problems are a major challenge for individuals with Prader-Willi syndrome (PWS), with significant impacts on quality of life and independence for both the person with PWS and their family. In 2015, FPWR conducted a two-day workshop bringing together approximately 45 top mental health researchers and clinicians from around the world to discuss behavior and mental health in PWS. The goal of the workshop was to develop a strategy for moving the science in the area forward. As part of this strategy, 10 recommendations were developed to advance mental health research and treatments for people with PWS (see article, Prader-Willi syndrome mental health research strategy workshop proceedings: the state of the science and future directions). Progress on these 10 recommendations is summarized below. A downloadable PDF of these recommendations is also available.
Mental health and behavioral problems are a major challenge for individuals with Prader-Willi syndrome (PWS), with significant impacts on quality of life and independence for both the person with PWS and their family. In 2015, FPWR conducted a two-day workshop bringing together approximately 45 top mental health researchers and clinicians from around the world to discuss behavior and mental health in PWS. The goal of the workshop was to develop a strategy for moving the science in the area forward. As part of this strategy, 10 recommendations were developed to advance mental health research and treatments for people with PWS (see article, Prader-Willi syndrome mental health research strategy workshop proceedings: the state of the science and future directions). Progress on these 10 recommendations is summarized below. A downloadable PDF of these recommendations is also available.
It is exciting to note that there has been a lot of activity in this area in the few years since the workshop, with several research studies underway, and a number of articles published on key areas, some of which are FPWR supported, and some of which are funded by other agencies. A brief summary of the work, organized by each of the 10 Recommendation, and links to the published articles is listed below:
Recommendation 1:
Obtain longitudinal and natural history data on mental health in PWS, including the behavioral and psychiatric components of the PWS phenotype.
Understanding the frequency, onset, and precipitating factors for mental illness in PWS is critical to understanding the scope and designing effective interventions. Since the Workshop, several new studies have been conducted to better define risk of mental illness in PWS, and propose models have been developed to achieve a better understanding of the psychopathological features in adults with PWS. Among the recent papers, several have characterized mental health challenges of PWS populations in different countries.
A group of experienced PWS clinicians in France characterized behavioral profiles in 150 adults with PWS, considering age, genetic subtype, and gender. A model to characterize psychopathological features in adults with Prader-Willi syndrome. Thuilleaux et al. 2017 They group patients into 4 major categories with respect to mental health challenges, including a “Basic” Profile (55% of individuals), “Impulsive” Profile (19% of individuals); “Compulsive” Profile (7% of patients) and “Psychotic” Profile (19% of individuals). Understanding the factors that impact which category a person with PWS falls in to will help mental health experts anticipate problems and develop more tailored interventions.
Dr. Shriki-Tal and colleagues in the PWS Multidisciplinary Clinic in Jerusalem studied psychiatric diagnoses and quality of life in their patients, age 12 and older. Psychiatric disorders in a cohort of individuals with Prader–Willi syndrome Shriki-Tal et al 2017 Most of the 53 individuals in this study had at least one behavioral/psychiatric challenge, with disruptive behavior and obsessive-compulsive disorder being most common. The incidence of psychosis was lower than some earlier studies, at slightly over 10%.
In the US, a study of 72 adults in residential care, revealed that anxiety disorder was common, occurring in 38% of individuals with PWS, while 23% of residents had experienced psychosis. A group in Japan examined behavior at different ages in young adults and adults with PWS, and found that problematic behaviors were higher in young adults compared to individuals over the age of 30, suggesting that challenging behavior may decline with continued maturation.
Finally, Dr. Hokken-Koelega and her team examined psychiatric symptoms in 61 children with PWS (ages 7-17) in the Netherlands. In their population, two children who had experienced psychosis were successfully treated with psychiatric medications, and no new cases were diagnosed during the two-year period of the study. Psychiatric disorders in children with Prader-Willi syndrome-Results of a 2-year longitudinal study. Lo et al.
Common themes across all of these population studies includes a high incidence of behavioral issues such as oppositional behavior, anxiety and OCD in persons with PWS, with psychiatric illness also occurring at considerably higher frequency in PWS than the typical population. Gender and genetic subtype differences were generally consistent with previous studies, which have suggested that those with PWS by UPD may be at a higher risk of developing psychosis, and that males are more prone to impulsive and aggressive behavior, but overall these associations were not as strong as some earlier studies indicated. The rate of mental health problems varied study to study, but it is clear that all individuals with PWS are at risk and should be carefully monitored. In addition longer, multinational studies are needed to fully understand risk factors as well as protective factors for mental illness.
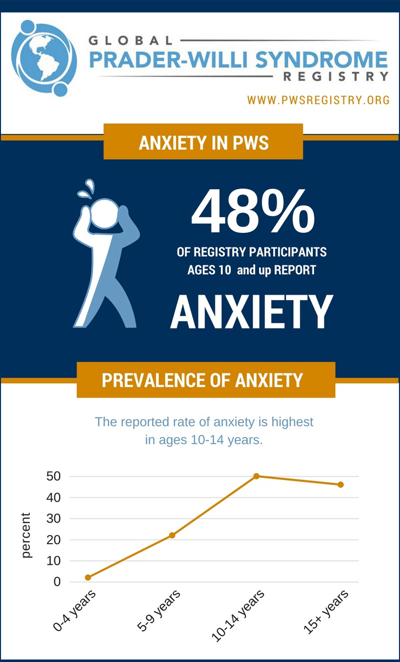
To this end, the Global PWS Registry is an important tool to understand behavior and mental health of a large PWS population over time. To date, more than 150 participants/caregivers have completed the behavior and mental health surveys in the Registry. These surveys are helpful in characterizing behavioral challenges, personality strengths, and mental illness. One of the most frequently reported behavioral challenges in Registry participants is anxiety, with differences in occurrence across age groups and genetic subtype. Current treatments for anxiety and other challenges include medications and behavior therapies often used in typically developing populations, but new treatments are on the horizon, which may be more effective in individuals with PWS who struggle with these challenges (e.g., oxytocin, carbetocin, CBD – see current PWS clinical trials list. To continue to strengthen the value of the Registry data, we encourage families to enroll their loved one with PWS in the Registry, and update their Behavior & Psychological history survey annually.
Recommendation 2:
Develop effective outcome measures for PWS mental health treatment studies.
In late 2015 FPWR launched the PWS Clinical Trials Consortium (PWS-CTC) to encourage collaboration and leverage the expertise and perspective of stakeholders from universities, patient organizations, and pharmaceutical companies to address the unmet scientific, clinical and regulatory needs of clinical trials for PWS. The Consortium aims to develop “outcome measures” to assess treatment benefits for new drugs and non-drug interventions targeting behavioral/mental health symptoms common in PWS, as well as hyperphagia (excessive appetite). The PWS-CTC is made up of several working groups, each addressing a different clinical trial challenge specific to PWS. The Behavioral Biomarkers Working group, composed of experts in PWS behavior analysis and clinical trials, has been very active over the last 2 years working to develop brief measures of behavioral issues in PWS (e.g., anxiety, tantrums, rigidity) to use in clinical trials of new medications and non medication interventions. FPWR is actively advancing the goals of this Working group and exploring new approaches (e.g., web-based and mobile technology methods) to monitor and characterize behavior in PWS. Look for updates on how you can help in the development and testing of new instruments to assess anxiety, rigidity, PWS personality attributes, and issues related to the food environment through the Global PWS Registry. Having broad participation by members of our PWS community will ensure that these new assessment tools are as strong and useful as possible.
Recommendation 3:
Determine the influence of weight management, hormones, and environment on mental well being over the PWS life course.
 The Global PWS Registry is key to achieving the goals of this recommendation as it will provide cross-sectional and longitudinal data to examine links between mental health, hyperphagia, weight, medication and environment. In addition, a number of specialized multidisciplinary PWS clinics at major academic medical centers follow individuals over many years, and the continued work of these researchers and medical professionals will be invaluable. Fostering opportunities to share information through publications, workshops, meetings and web-based educational meetings is vital for facilitating the dissemination of the clinical experiences so that it can reach as many individuals as possible.
The Global PWS Registry is key to achieving the goals of this recommendation as it will provide cross-sectional and longitudinal data to examine links between mental health, hyperphagia, weight, medication and environment. In addition, a number of specialized multidisciplinary PWS clinics at major academic medical centers follow individuals over many years, and the continued work of these researchers and medical professionals will be invaluable. Fostering opportunities to share information through publications, workshops, meetings and web-based educational meetings is vital for facilitating the dissemination of the clinical experiences so that it can reach as many individuals as possible.
With respect to specific studies that address this goal, new studies published since the Workshop indicate that hormone replacement improves health and quality of life in adults with PWS. This includes use of growth hormone in children and adults with PWS, as well showing benefits of testosterone replacement in males with PWS. There are some indications that weight management has improved over the past several years, and this appears to be positively impacting physical activity, which is, in turn, known to improve mental health.
Recommendation 4:
Apply diverse research methods to advance mechanistic research on the neurobiology underlying mental health and behavioral issues in PWS.
A variety of scientific disciplines (e.g., molecular studies, brain imaging) have been applied to better understand the root cause of mental illness in PWS since the 2015 workshop – an important step in being able to develop interventions to mitigate mental health problems. New technologies – from “neurons in a dish” (neurons grown in the laboratory, derived from stem cells) to advances in brain imaging - have accelerated this work.
One perplexing aspect of mental illness in PWS is the difference in risk between those with PWS by deletion and those with PWS due to maternal uniparental disomy (UPD) or imprinting defect (ID). While all individuals with PWS are at high risk for behavioral difficulties and mental health problems, individuals with PWS by UPD or ID are specifically at higher risk of developing psychosis. Several papers published since the Workshop advance our understanding of these differences and propose factors that may be underlying these issues. In addition, there have been new findings to explain how PWS brain development might contribute to behaviors that affect many individuals with PWS, such as obsessive compulsive disorder, oppositional behaviors, and temper outbursts.
Among theses newer studies, several examine brain structure and connectivity in children and adults with PWS (see below - Manning, Rice Lukoshe, Forster). These papers show that there are regions of the brain that are structurally different in individuals with PWS compared to typically developing individuals, in both the white (Rice) and grey matter (Manning) of the brain. These changes are in areas that are thought to be important in modulating attention, emotion regulation and sensory function. In addition, there may be unique differences in the brains of individuals with UPD, which may be contributing to the increased risk of psychosis in this subgroup (Lukoshe). Finally, changes in a particular set of neurons (Von Economo) may contribute to challenges in social functioning in PWS (Forster). Understanding these anatomical changes and differences is important because there are current efforts in the neurobiology field to use brain imaging techniques to improve individual prediction of a transition to psychosis in high risk individuals (also, Grazioplene and co-workers). These imaging studies will be further informed by large scale efforts to understand variation in brain structure in typical individuals, and individuals at risk for mental illness, such as work being done in the NIH Brain Initiative.
Manning,K.E., Tait, R., Suckling,J., Holland, A.J. Grey matter volume and cortical structure in Prader-Willi syndrome compared to typically developing young adults. Neuroimage Clin. 2018; 17: 899–909.
LJ Rice, J Lagopoulos, M Brammer, Einfeld, S.L. Microstructural white matter tract alteration in Prader‐Willi syndrome: A diffusion tensor imaging study. Am J Med Genet C Semin Med Genet. 2017 Sep;175(3):362-367. doi: 10.1002/ajmg.c.31572.
A Lukoshe. Aberrant white matter microstructure in children and adolescents with the subtype of Prader–Willi syndrome at high risk for psychosis.Schizophr Bull. 2017 Sep 1;43(5):1090-1099. doi: 10.1093/schbul/sbx052
Forster, J., Varghese M., Hof, P. Stereology of Von Economo Neurons (VENs) in Anterior Cingulate Cortex (ACC) and Insula of Post Mortem Brains From Persons With Prader-Willi Syndrome (PWS): A Preliminary Report. Child & Adolescent Psychiatry. 2017 Oct. 56(10):S22
There have also been discoveries about changes in brain chemistry and neuronal function that may be contributing to behavioral symptoms in PWS. Among these, the activity of specific receptors may be altered by the loss of certain PWS region genes (Falaleeva, Stamm, see references below) and may differ between individuals with PWS by deletion vs. UPD (Krishnadas). Rice et al., found that the levels of one of the main neurotransmitter chemicals of the brain, “GABA”, is reduced in those with PWS, which may underlie some of the behavioral issues such as temper outbursts and depression. Finally, Bochukova and colleagues examined molecular changes in PWS brain tissue and found an increase in inflammation signatures, and decreases in certain brain growth factors (e.g., BDNF). These findings suggest new targets for drug therapies that might work to normalize the overall brain chemistry and function in PWS. A comprehensive review of many of the new findings was published early in 2018, by the Cambridge developmental psychiatry group, and includes a model of potential mechanisms of psychosis in PWS (Aman). Again, these PWS specific initiatives are complemented by progress in the field in general, where new studies are mapping molecular changes in different psychiatric disorders and other studies have shown the promise of using an understanding of metabolic changes in the brain to predict the onset of mental illness.
Falaleeva, et al. SNORD116 and SNORD115 change expression of multiple genes and modify each other's activity.Gene. 2015 Nov 10;572(2):266-73. doi: 10.1016/j.gene.2015.07.023.
Stamm, et al. The activity of serotonin receptor 2C is regulated by alternative splicing. Hum Genet. 2017 Sep; 136(9): 1079–1091. doi: 10.1007/s00439-017-1826-3
Krishnadas R, et al. Brain-stem serotonin transporter availability in maternal uniparental disomy and deletion Prader-Willi syndrome. Br J Psychiatry. 2018 Jan;212(1):57-58. doi: 10.1192/bjp.2017.7.
Rice, Einfeld, et al.: Reduced gamma-aminobutyric acid is associated with emotional and behavioral problems in Prader-Willi syndrome.Am J Med Genet B Neuropsychiatr Genet 2016 Dec;171(8):1041-1048. doi: 10.1002/ajmg.b.32472.
Bouchukova, et al.:A Transcriptomic Signature of the Hypothalamic Response to Fasting and BDNF Deficiency in Prader-Willi Syndrome. Cell Reports. 2018 Mar 27;22(13):3401-3408. doi: 10.1016/j.celrep.2018.03.018.
Aman, Manning, Whittington & Holland. Mechanistic insights into the genetics of affective psychosis from Prader-Willi syndrome.Lancet Psychiatry. 2018 Apr;5(4):370-378. doi: 10.1016/S2215-0366(18)30009-9.
Recommendation #5 Identify markers (neurobiological, genetic, psychological, environmental) of impending mental illness and characterize features of the prodromal phase (especially psychosis) in PWS, in order to reduce and/or prevent psychiatric illness.
Mental health researchers are starting to focus on the early detection and possible prevention of the onset of serious mental illness, especially for people who are identified to be at high risk. The PWS population is an ideal population for such studies since there is a high risk for mental illness, including psychosis. This blog summarizes some of the latest advances in the area of predicting and preventing onset of mental illness, including the work of Dr. Carrie Bearden. Dr. Bearden, a participant at the PWS Mental health research workshop, is currently funded by FPWR to develop assessment strategies for predicting impending mental illness in PWS, this is the first study in this area and is an important first step to treatment and possible prevention. Preliminary results for this study indicate that of the 87 participants who have completed the self or parent report screening questionnaire on early psychiatric and psychotic like symptoms called the Prodromal Questionnaire, about 40% endorse symptoms that reflect possible early psychiatric issues. Significant distress related to these symptoms was reported in about 1/3 of the sample. These preliminary results suggest that unusual thinking and possible early psychiatric symptoms are reported for a significant proportion of teens and adults with PWS.
Identifying the prodromal or early signs of psychosis in PWS will enable early intervention and treatment, which has been shown to result in better mental health outcomes. In addition to medication, there is hope for non-pharmacologic treatment to be effective in treating symptoms of psychiatric illness in PWS, including family therapy focused on stress reduction, vagus nerve stimulation, and cognitive behavioral therapy for psychosis. The results from Dr. Bearden's study will pave the way for a larger prospective study, and transform our understanding of mental illness in PWS. Additionally such studies lay the groundwork for future exploration of potential early intervention strategies for those individuals with PWS who are exhibiting the early signs of psychiatric issues.
Recommendation 6:
Facilitate further research on oxytocin and vasopressin in PWS in order to refine the timing and dosing of oxytocin.
The PWS Mental Health Research Strategy Workshop generated a lot discussion on the topic of Oxytocin and PWS in the session entitled – The Oxytocin Conundrum. Since the workshop, several research projects, clinical trials and some exciting research collaborations among the workshop participants have occurred. The project 'Oxytocin and the autonomic nervous system in Prader-Willi syndrome was the product of collaborative efforts stemming from the PWS mental health workshop.
Dr. Lauren Rice and colleagues have also collaborated on an excellent review of PWS Oxytocin clinical trials research to date. Briefly the article summarizes the published findings of 5 previous clinical trials of oxytocin in PWS. Four of these previous studies reported that oxytocin showed some improvement in behavior. However, there were some important limitations in each of the studies that likely affected the findings (e.g., lack of control group or validated measures of behavior/hunger). Future and current trials are designed to address these limitations with the aim of obtaining more solid data and understanding of the potential role of intranasal oxytocin in improving symptoms in PWS. (see Rice, L. Einfeld, E. Hub, N. Carter, S. A review of clinical trials of oxytocin in Prader–Willi syndrome. Current Opinion in Psychiatry: 2017).
Two small clinical trials of oxytocin in infants and young children with PWS have also been published in the last 2 years. These studies showed improvements in some of the parameters measured in the participants with PWS (e.g., improvements in feeding in infants, social responsiveness, repetitive behaviors).
Tauber M, et al. The Use of Oxytocin to Improve Feeding and Social Skills in Infants With Prader-Willi Syndrome. Pediatrics. 2017 Feb;139(2). pii: e20162976. doi: 10.1542/peds.2016-2976.
Miller JL, Tamura R, Butler MG, Kimonis V, Sulsona C, Gold J, Driscoll DJ. Oxytocin treatment in children with Prader-Willi syndrome: A double-blind, placebo-controlled, crossover study. Am J Med Genet A. 2017 May;173(5):1243-1250. doi: 10.1002/ajmg.a.38160.
Another small, recently published study showed positive impacts of a drug that is molecularly similar to oxytocin, ‘carbetocin’ in PWS, Dykens et al., This study showed that carbetocin reduced hyperphagia as well OCD behaviors in children (aged 10-18 Yrs.)with PWS when children received the drug three times a day for two weeks, setting the stage for a larger, longer Phase 3 clinical trial to further assess efficacy (expected in Fall 2018).
There are 5 additional ongoing/recently completed clinical trials of Oxytocin in PWS:
Follow-up of Prader Willi Syndrome Infants Treated by Oxytocin and Comparison With Not-treated Infants. ClinicalTrials.gov Identifier: NCT03081832. University Hospital, Toulouse. Principal Investigator: Maithe Tauber, M.D. (2017, currently ongoing)
Effects of Intranasal Administration of Oxytocin in Adults With Prader-Willi. ClinicalTrials.gov Identifier: NCT02804373. University Hospital, Toulouse. Principal Investigator: Maithe Tauber, M.D. (2016, completed).
Intranasal Oxytocin for Infants With Prader-Willi Syndrome. ClinicalTrials.gov Identifier: NCT03245762. University of Florida. Principal Investigator: Jennifer Miller, M.D (2017-2018, completed).
Oxytocin vs. Placebo for the Treatment of Hyperphagia in Children and Adolescents With Prader-Willi Syndrome. ClinicalTrials.gov Identifier: NCT02629991. This study also examines impact on PWS behaviors as secondary measures. Principal Investigator: Eric Hollander, M.D (2017 completed)
Intranasal Oxytocin vs. Placebo for the Treatment of Hyperphagia in Prader-Willi Syndrome: Ages 5 to 18 yrs. ClinicalTrials.gov Identifier: NCT03197662. This study will also examine impact on various PWS behaviors as secondary measures. Principal Investigator: Eric Hollander, M.D (2018, recruiting)
 New clinical trials examining the use of oxytocin and its analogs are on the very near horizon. Sign up for the FPWR Clinical Trials Alert to stay informed about upcoming trials in PWS and get the latest updates.
New clinical trials examining the use of oxytocin and its analogs are on the very near horizon. Sign up for the FPWR Clinical Trials Alert to stay informed about upcoming trials in PWS and get the latest updates.
In addition to these clinical studies, FPWR has been supporting studies to better understand the mechanism(s) by which oxytocin may improve symptoms of PWS, and specifically how the delivery of oxytocin (orally vs. nasal) may mediate its effects.
Dr. Hammond at Florida State University is exploring this aspect in mouse models. The results of this work will help define mechanisms driving effectiveness of Oxytocin as a therapy for the feeding and social challenges seen in PWS.
Another study by Dr. Muscatelli is focused on understanding the mechanisms of oxytocin action in animal models of PWS, to guide the development of oxytocin interventions for humans.
Dr. Driscoll is examining in greater depth the factors that determine why some individuals with PWS seem to respond strongly to oxytocin treatment, while others show less effect.
Overall, oxytocin continues to hold therapeutic promise for PWS, and the work of many investigators will be needed to understand how to optimize its use and efficacy for individuals with the disorder.
Recommendation 7:
Further assess autonomic nervous system (ANS) function in PWS to determine if the polyvagal theory and treatments related to that theory help explain or improve temper outbursts, anxiety and other behavioral problems.
Several research projects and collaborations have been initiated and are moving forward focused in this area since the PWS mental health workshop.
One key aspect of the autonomic nervous system is the vagus nerve, which is thought to play an important role in hunger, digestion, anxiety and behavior. The vagus nerve is involved in the flight or fight response and provides the gateway between the two parts of the autonomic nervous system (i.e., parasympathetic and sympathetic nervous system). Dysfunction in this important pathway has been hypothesized to underlie symptoms in conditions such as autism, eating disorders, anxiety disorders and gastroparesis. In early 2016, a paper exploring this pathway in PWS was published by Dr. Tony Holland’s research group reporting on the use of Vagus nerve stimulation (VNS) in PWS (see Manning et al., Novel insights into maladaptive behaviors in PWS. J Intellect Disabil Res. 2016 Feb; 60(2): 149–155. doi: 10.1111/jir.12203). This paper reported on unexpected improvements in challenging behaviors during a trial of VNS in 3 adults with PWS. This was a pilot study had been designed to focus on hyperphagia (which was not significantly improved by VNS) but the degree of the improvement in challenging behavior was considered remarkable in these adults with PWS. Over the last 2 years, Dr. Holland’s research team has gone on to conduct a larger trial to specifically examine the impact of VNS on behavior in PWS. This study is not yet completed but we are looking forward to hearing about the results in the next year. For further details see the blog: Will Vagus Nerve Stimulation Effectively Treat Behavior in PWS?
Expanding the exploration of issues in the autonomic nervous system and potential impact on PWS, Dr. Stephen Porges, who was a keynote speaker at the PWS mental health research workshop, has been exploring the application of his Polyvagal theory to PWS. The polyvagal theory focuses on the flight, fight or freeze responses in humans and how mechanisms controlling these processes may not be working properly in certain conditions. Dr. Porges is collecting data exploring this with a project entitled Optimizing the Social Engagement System in Prader-Willi Syndrome: Insights From the Polyvagal Theory. (2017-2018, recruiting)
Additionally another study is ongoing focused on examining aspects of the polyvagal theory by measuring respiratory sinus arrhythmia (RSA) in PWS. RSA is another way to measure vagus nerve activity. This study will assess whether RSA abnormalities exist in PWS and how such abnormalities may relate to emotional and behavioral issues as well as oxytocin/vasopressin abnormalities in PWS. This study is important, as it will help to identify some of the possible physiological underpinnings and potential mechanisms of maladaptive behaviors of PWS.
Recommendation 8:
Modify and test the efficacy of state of the art behavioral interventions for anxiety, temper outbursts and social challenges in PWS.
Three exciting projects have started since the PWS mental health research workshop. The researchers spearheading these projects were key participants in the workshop.
Drs. Elisabeth Dykens and Elizabeth Roof at Vanderbilt University are conducting a 2-year project on social skills intervention aimed at developing an online curriculum specific for teens and young adults with PWS. This curriculum is focused on helping teens and young adults with PWS develop tools to address social challenges that are commonly seen in PWS (e.g., emotional regulation, theory of mind). One aspect of this study that is unique and addresses a potential challenge treating people with a rare disease is that it an online interactive group so people with PWS from all over the United States, from Alaska to Seattle to Boston and beyond, have been able to participate.
Another exciting and innovative project is underway focusing on an intervention for temper outbursts in PWS. Dr. Stewart Einfeld and his team at the University of Sydney are currently recruiting for their pilot project focused on developing a portable mindfulness intervention to address temper outbursts and anxiety in PWS.
Finally, Dr. Kate Woodcock and her team have conducted several studies showing that people with PWS have trouble with change (“task switching”) and this can trigger tantrums and other challenging behaviors. See - Haig, E.L. Woodcock., K.A. Rigidity in routines and the development of resistance to change in individuals with Prader–Willi syndrome. J Intellect Disabil Res. 2017 May;61(5):488-500. doi: 10.1111/jir.12368. Dr. Woodcock and her team are currently focused on developing a web-based video game intervention to evaluate whether children with PWS can learn to better ‘task-switch’ with practice and whether this has an impact on behavioral issues in PWS.
Recommendation 9:
Define parental/caregiver stress, develop interventions to reduce caregiver stress and determine effects of reducing caregiver stress on child functioning.
There has been work over the last few years to define caregiver stress in parents who care for their child with PWS. This stress, which is referred to as ‘caregiver burden’ in the medical literature, likely is due to the unique combination of hyperphagia and behavioral challenges in individuals with PWS. The findings of a recently published study of PWS caregivers residing in the US documented the high levels of ‘caregiver burden’ and highlighted the critical unmet need for support for caregivers of individuals with PWS. In this study, rates of caregiver burden were highest for those caregivers whose children were in the adolescent and young adult PWS age groups. The timing of increased hyperphagia and the possible development of psychiatric/behavioral symptoms in PWS that often occurs during that time period could explain this finding. However, further research needs to be conducted to better understand the factors that influence caregiver stress in PWS and how this may change over time.
In 2016, Lopez-Bastida et al. examined caregiver stress and economic and social burden in PWS, across several European countries. This study found that PWS caregivers in some of the countries such as Spain, the UK and France, had very high caregiver burden scores similar to the study mentioned above conducted with US caregivers.
In 2017, FPWR conducted a webinar focused on caregiver stress that included a discussion of the results of research in this area as well as suggestions to help caregivers, and information about an upcoming study focused on caregivers that will advance clinical trials for PWS. See 2 different blogs on this topic:
- Studies show PWS caregiver stress can and should be addressed
- Bringing PWS caregiver perspectives into the development of therapies
FPWR is currently encouraging researchers to submit proposals focused on interventions for PWS caregivers to evaluate the efficacy of different approaches to reduce caregiver stress, and the impact on the child with PWS. It will be key to develop an approach that is realistic, can be applied to most families; and will be motivating for families to participate in. Stay tuned for new developments in this area on the horizon.
Recommendation 10:
The involvement and engagement of parents, families and caregivers (both family and professional) at all levels is critical to advancing knowledge and treatment. This should also include input from youth and adults with PWS.
The input of individuals with PWS and their families is critical, so that we can pursue those issues of highest importance to the patient community. Based on input to date, these are some things that are high on our list:
- Document the ‘PWS patient experience’ so that the voice of our loved ones with PWS can be heard. A project is currently being developed as part of the PWS Clinical Trial Consortium to incorporate the perspective of adolescents and adults with PWS into discussions about unmet medical needs, treatment preferences and patient experience.
- Develop family and physician guides for mental health issues, especially mental health crises by collecting stories from families and clinicians who have been working with these conditions in their loved ones/patients. The goal of this project is to develop a brief document to guide families/caregivers about ‘what to look for’ and ‘what to expect’ regarding potential mental health symptoms in PWS.
- Develop short-term management strategies for families to help address their stress, improve coping and help create resilience for the PWS journey.
Finally, the Global PWS Registry is a critical resource to advance mental health research in particular and clinical trials in PWS in general. The Registry is compiling data on mental health and other challenges in PWS over the lifespan. Everyone needs to do the registry so it can speak to the range of strengths, challenges and symptoms that our loved ones with PWS experience.
We welcome your thoughts on these, and other issues that are important to you – please provide your input by emailing me here.









